Understanding Private Healthcare: Benefits and Challenges Explained
Outline and Context: How Insurance, Telemedicine, and Patient Care Interlock
Private healthcare can feel like a three-gear mechanism: insurance funds the engine, telemedicine extends its reach, and patient care measures whether the machine runs smoothly. Understanding how these elements mesh helps you evaluate trade-offs, from monthly costs to clinical outcomes. This article begins with a roadmap, then moves into deeper analysis with practical examples and comparisons across different systems and settings. The aim is to equip readers—patients, families, and purchasers—with a reliable framework for decision-making rather than slogans or vague promises.
Here is the structure we will follow in the pages ahead, including what to expect from each part and how to apply the insights immediately to your situation:
– Section 1 (this section): A narrative outline and orientation, clarifying terms and relationships among insurance, telemedicine, and patient care.
– Section 2: Insurance in private healthcare—how coverage design affects access, bills, and behavior; what to look for in policies; ways to mitigate surprise costs.
– Section 3: Telemedicine—where it shines, where it falls short, and how to verify quality; hybrid models that blend virtual and in-person care.
– Section 4: Patient care—safety, outcomes, and experience; staffing, continuity, and data sharing; how private settings organize services.
– Section 5: A practical roadmap—actionable steps for patients and purchasers to balance convenience, cost, and quality.
Two themes thread through every section. First, incentives matter: cost-sharing, provider payment models, and network design shape behavior, wait times, and continuity. Second, infrastructure matters: digital records, appointment logistics, and service integration largely determine whether care feels coordinated or fragmented. Throughout, we will reference widely reported patterns—for instance, in many high-income countries, private sources finance roughly 20–30% of health spending, though the mix varies—and we will draw on recent telemedicine adoption trends, which surged during the pandemic and settled at a steady share of visits in subsequent years. By the end, you should be able to match your priorities to realistic options and anticipate the knock-on effects of each choice.
Insurance in Private Healthcare: Access, Costs, and Trade-offs
Insurance is the entry ticket to much of private healthcare, but the rules on the ticket are as important as admission itself. Policies typically combine premiums (what you pay regularly), deductibles (what you pay before coverage applies), co-payments or coinsurance (your share per service), and out-of-pocket maximums (the ceiling on your annual spending). Network design—preferred providers or open access—often influences price and appointment availability more than people realize. Narrow networks may offer lower premiums but restrict choices; broader networks expand options but can come with higher monthly costs.
Across many high-income systems, private sources account for a significant minority of total health spending, commonly via voluntary insurance and direct out-of-pocket payments. That share can shift with policy reforms, demographic pressures, and employer purchasing strategies. Two practical patterns matter for consumers: first, cost-sharing nudges patients to compare options but can also deter necessary care if set too high; second, negotiated rates can make the “list price” of services misleading. A diagnostic scan might appear costly at face value, yet contracted rates often reduce the bill substantially—if you stay in-network and pre-authorize services where required.
When comparing policies, look beyond headline premiums. Scrutinize specifics that can quietly multiply costs or administrative hassle:
– Referral requirements: Some plans require a primary clinician’s referral for specialty care; skipping this step can void coverage for that visit.
– Prior authorization: Complex therapies, imaging, or elective procedures may need approval; timelines and criteria vary by plan.
– Drug formularies and tiers: Medication coverage differs widely; out-of-pocket exposure hinges on tier placement and generic availability.
– Out-of-area rules: Coverage for travel or temporary residence can be limited or conditional.
Consider the “behavioral” side of insurance design. Lower co-pays for preventive services tend to increase uptake of screenings and vaccinations, contributing to earlier detection and fewer complications. Value-based arrangements—where providers share accountability for outcomes and costs—can encourage coordination and reduce duplicative tests. However, incentives can cut both ways: very narrow networks or strict authorization rules can slow access or lead to “care shopping fatigue.” A pragmatic approach is to map your likely healthcare needs for the coming year—chronic conditions, planned surgeries, expected medications—and project spend under two or three policy options. This exercise turns abstract terms into concrete trade-offs and often reveals that a slightly higher premium can be more affordable overall if it meaningfully reduces deductibles and protects against volatility.
Telemedicine as a Care Channel: Opportunities, Limits, and Quality Standards
Telemedicine has matured from a convenience to a core channel in private healthcare, particularly for primary care, behavioral health, and routine follow-ups. During the early pandemic period, virtual visits surged dramatically; since then, utilization has stabilized at a meaningful share of outpatient encounters in many regions, often ranging from single-digit to low double-digit percentages depending on specialty. The appeal is clear: lower travel time, faster scheduling, and the ability to loop in caregivers from different locations. For clinicians, virtual tools can streamline check-ins, medication reviews, and triage decisions that determine whether an in-person exam is truly necessary.
Yet not every clinical question belongs on a screen. Limitations include the inability to perform hands-on exams, variable connectivity, and environmental distractions that can impede accurate assessment. Hybrid models—virtual-first intake with targeted in-person follow-up—tend to work well, pairing convenience with physical examination when needed. Remote patient monitoring devices for blood pressure, glucose, or oxygen saturation can extend telemedicine’s reach, but they depend on reliable equipment and data interpretation workflows. Privacy and security practices are also essential; encryption, audit logs, and consent routines help maintain trust and regulatory compliance.
Quality in telemedicine can be evaluated with familiar yardsticks, adapted for a digital context. Consider the following markers when judging virtual care programs:
– Clinical appropriateness: Clear protocols that specify which symptoms or conditions are suitable for virtual visits and when to escalate to in-person care.
– Access metrics: Same-day or next-day availability, extended hours, and minimal wait times within a scheduled slot.
– Continuity and records: Integration with your longitudinal medical record so information flows to all relevant clinicians.
– Patient-reported outcomes: Short symptom scales and satisfaction measures fielded after visits to track progress and experience.
– Safety monitoring: Processes for urgent symptoms, identity verification, and medication reconciliation.
For private providers, telemedicine can reduce missed appointments and optimize clinician schedules, but throughput should not trump quality. Effective programs anchor virtual visits in standardized documentation, decision support, and easy pathways to imaging, labs, or urgent evaluation when indicated. Measured carefully, telemedicine has shown comparable outcomes to in-person care for many conditions such as uncomplicated infections, routine mental health follow-ups, and chronic disease check-ins. The enduring value lies in its role as one component of an integrated system—fast for simple needs, confident in knowing when to say, “Please come in today.”
Patient Care, Safety, and Experience: What Truly Changes at the Bedside
The promise of private healthcare is often described in terms of speed and amenities, but the heart of patient care is still safety, clinical outcomes, and respectful communication. Shorter wait times and quieter facilities are meaningful, yet they matter most when paired with robust clinical governance: evidence-based protocols, reliable diagnostics, and skilled multidisciplinary teams. In practice, what improves care is less the color of the waiting room and more the choreography behind the scenes—how pharmacists, nurses, physicians, and therapists coordinate around a shared plan.
Safety culture is visible in small details. Accurate medication reconciliation prevents interactions; surgical checklists reduce preventable harm; infection prevention routines protect patients and staff. Private settings frequently invest in diagnostics and scheduling systems that compress the time from referral to test to result, which can improve outcomes in time-sensitive conditions. Still, vigilance is essential: fragmented records and out-of-network referrals can create gaps. That is why integrated digital records and clear discharge summaries matter so much; they are not paperwork, but patient safety tools.
From the patient’s perspective, three levers consistently shape experience and outcomes:
– Communication: Clear explanations, teach-back methods, and written instructions reduce confusion and readmissions.
– Continuity: Seeing the same clinicians builds trust and speeds decision-making; where continuity is not possible, handoffs must be crisp.
– Access to services: On-site imaging, timely lab slots, and pharmacy coordination keep care moving and limit loss to follow-up.
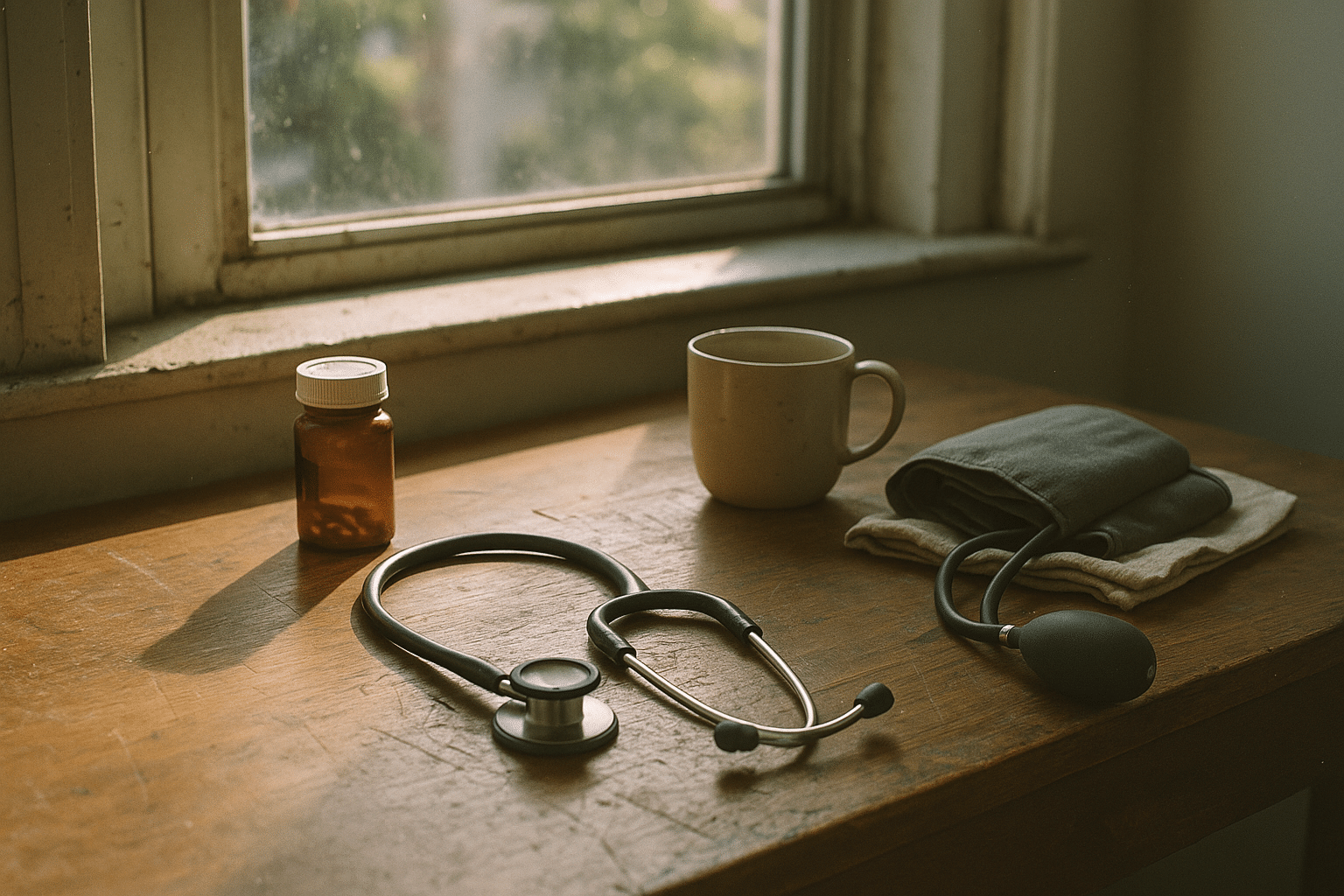
Consider a patient with newly diagnosed hypertension. In a coordinated private setting, the initial visit might include baseline labs, home blood pressure monitor setup, and a virtual follow-up booked before the patient leaves. Pharmacists reconcile medications the same day and reinforce lifestyle advice. Two weeks later, the telemedicine check-in reviews home readings and adjusts therapy; an in-person exam confirms response and checks for side effects. The outcome is not just a lower number on a screen but fewer headaches, better sleep, and confidence in the plan.
Measuring what matters makes these improvements durable. Track readmissions, unplanned returns to the emergency department, adherence to guidelines, and patient-reported outcome measures for targeted conditions. When these indicators move in the right direction, it suggests that the experience patients notice—friendly staff, shorter waits—rests on real clinical progress rather than mere polish.
Conclusion: A Practical Roadmap for Patients and Purchasers
Choosing private healthcare is ultimately about matching your needs and values to a system’s strengths. Insurance defines the financial runway; telemedicine extends reach and convenience; patient care practices determine whether outcomes and safety truly improve. The path forward is most effective when it is intentional and data-informed, not improvised. Below is a concise roadmap you can use to translate principles into action over the next twelve months.
– Map your likely needs: List chronic conditions, planned procedures, and routine medications; estimate annual utilization to compare insurance options realistically.
– Stress-test coverage: Check deductibles, out-of-pocket caps, referral and authorization rules, and out-of-area benefits; confirm drug tiers for current prescriptions.
– Assemble your team: Identify a primary clinician who coordinates care; confirm that preferred specialists and key facilities are in-network.
– Build a hybrid care plan: Use telemedicine for follow-ups, medication reviews, and quick triage; reserve in-person visits for physical exams, complex symptoms, or procedures.
– Track outcomes: Set a handful of metrics—symptom scores, blood pressure averages, days missed from work or school—to monitor progress against your goals.
For families, predictability matters as much as headline price. Policies with slightly higher premiums may offer stability by lowering deductibles and streamlining access to frequent services like therapy, imaging, or routine consultations. For employers and other purchasers, value-based arrangements and integrated networks can reduce administrative friction and promote consistent quality, provided performance metrics are transparent and regularly reviewed. In all cases, keep records unified—bring discharge summaries, medication lists, and device readings to every visit, virtual or in-person, so that each clinician works from the same playbook.
The private healthcare landscape will continue to evolve as payment models, digital tools, and clinical standards advance. By clarifying your priorities, verifying coverage details, and embracing a hybrid care approach, you can capture the convenience and responsiveness that private systems often provide while safeguarding safety and outcomes. Think of it as good navigation: set your destination, study the route, and check your instruments along the way. With that discipline, you turn a complex market into a manageable plan that serves your health, your time, and your budget.